Muhammad Irfan ( Department of Psychiatry and Behavioural Sciences, Peshawar Medical College, Riphah International University, Islamabad. )
Jose Miguel Caldas de Almeida ( Faculty of Medical Sciences, Department of Mental Health, NOVA University of Lisbon, Compo Martires da Patria, Lisbon, Portugal. )
Uma Maheswari Irfan ( College of Applied Medical Sciences, Qassim University, Buraydah, Kingdom of Saudi Arabia. )
Usman Ahmad Raza ( Department of Community Health Sciences, Peshawar Medical College, Peshawar. )
Saeed Farooq ( Lady Reading Hospital, Peshawar. )
September 2015, Volume 65, Issue 9
Original Article
Abstract
Objective: To assess the knowledge and practices of general practitioners about diagnosis and treatment of schizophrenia and determine their association with clinical exposure to such cases in practice.
Methods: The cross-sectional study was conducted in Peshawar from August 2009 to December 2011 at the clinics of general practitioners enrolled with the provincial Health Regulation Authority. All the listed GPs were contacted and those consenting to participate were included. A semi-structured questionnaire was used to assess their knowledge and practices related to diagnosis and treatment of schizophrenia. They were categorised as having Good Knowledge/Practice, in this regard, when they responded to >60% of the questions correctly.
Results: Of the 135 general practitioners contacted, 114(84.5%) agreed to participate and represented the study sample. Of them, 61(53.5%) physicians did not treat any diagnosed case while 15(13.2%) treated more than 10(8.8%) annually. Only 6(5.3%) practitioners spent more than 30 minutes, while 22(19.3%) spent less than 10 minutes per patient. Besides, 14(12.3%) practitioners had good knowledge about schizophrenia diagnosis and treatment, while 100(87.7%) had poor or no knowledge. Similarly, 32(28.1%) practitioners had good practice skills regarding schizophrenia compared to 82(71.9%) having poor practice skills or no practice regarding schizophrenia. General practitioners who were not treating any patients with schizophrenia had lower knowledge and practice scores compared to those who were treating one or more patients with schizophrenia annually (p<0.001 each).
Conclusion: The knowledge and practice skills of general physicians were below average by medical standards regarding schizophrenia diagnosis and treatment.
Keywords: Knowledge, Practice, Schizophrenia, General Practitioner (GP). (JPMA 65: 937; 2015).
Introduction
Schizophrenia is a disorder involving chronic or recurrent psychosis and long-term decline in functional ability.1 It affects about 24 million people worldwide with more than 50% of these not receiving appropriate care and out of 90% of these reside in developing countries, Pakistan being one of them.2
The correct prevalence of schizophrenia in Pakistan is not known which prevents the making of national-level strategies to combat this incapacitating and burdensome illness. Taking in account the global prevalence and the draft of "Assessment of Health Status & Trends in Pakistan", the estimated prevalence of schizophrenia in Pakistan may be 1-2% in the general population.3
Schizophrenia, apart from affecting a person in terms of immense suffering, also affects the individual and the family with high levels of social burden and cost.4 These burdens may involve many factors, including characteristics of patients and caregivers; family size; economic status; role expectations; and illness-related beliefs.5
In 1990, the estimated loss in disability-adjusted life years (DALYs) due to schizophrenia and associated disorders was around 13 million representing almost 1% burden of the disease from all causes and was ranked 26th on the list. By 2020, schizophrenia is projected to be in 20th position with a DALYs loss of more than 17 million and accounting for 1.25% of the overall burden.6
Although schizophrenia is best treated in specialty clinics, but general practitioners (GPs) and primary care clinicians encounter the diagnosis in a variety of contexts, including initial presentation, evaluation of concurrent medical illness, provision of support to family members, management of medication side-effects and primary treatment; more so when specialty options are not available. Also, GPs offer people an easy and non-stigmatising access to healthcare.7 People with schizophrenia place significant demands on the primary care services.8 They consult more frequently than other patient groups, often for reasons unrelated to their mental illness and have high rates of attendance with physical complaints9 as they have high levels of psychological morbidity10 and make considerable demands on GP services.11
Most people with schizophrenia in low and middle income countries (LMICs) probably receive little or no formal care. One manifestation of this is very long duration of untreated psychosis in the first episode in these countries, i.e., 132 weeks.10 This poses a major public health problem considering that around 41.7 million people with schizophrenia may need care in LMICs.11 The GPs, therefore, have to play a crucial role in early diagnosis and management of schizophrenia. Like other developing countries, the number of psychiatrists for the diagnosis and treatment of schizophrenia is very low.12 Thus, Pakistan is a good case to advocate the importance of the role of GPs in this regards.13,14 They may help in treating the patients with an established diagnosis of schizophrenia13 as well as in identifying people in the early stages of psychosis14 and evidence suggests that schizophrenia if treated earlier has a better prognosis.15
Unfortunately, there are only a few studies that focus on the knowledge and practice of GPs in dealing with schizophrenic patients around the globe.16,17 None of these studies address this issue in LMICs. We, therefore, decided to conduct a study to assess the knowledge and practices of GPs about schizophrenia in a major urban centre to identify the gaps in knowledge and practice in service delivery, and also to determine the association of knowledge and practice scores with clinical exposure to schizophrenia cases in practice.
Subjects and Methods
The cross-sectional study was conducted in Peshawar from August 2009 to December 2011 at the clinic of GPs enrolled with the provincial Health Regulation Authority. Unlike UK and other countries, in Pakistan the GPs are not defined by their registration or after a specified period of training. For the purpose of this study a GP was defined as, "A licensed medical graduate who gives personal, primary and continuing care to individuals, families and a practice population irrespective of age, sex and illness".5
All the enlisted GPs were approached and those who gave consent to participate in the study were included after ethical approval was obtained by the review and ethical board of the Postgraduate Medical Institute, Lady Reading Hospital, Peshawar.
The GPs were requested to answer a semi-structured questionnaire consisting of three parts: General Information; Knowledge; and Practices related to schizophrenia. The questionnaire was based on an earlier seminal study.15 As the questionnaire was originally developed in Switzerland where the health system and GP practice differs markedly from that in Pakistan, the questionnaire was modified to reflect the practice and health services structure in Pakistan. However, the major domains, questions and content was retained. The 17-item questionnaire consisted of 6 demographic questions and of the 11 questions that assessed knowledge and practice, 7 related to symptoms of schizophrenia, early warning signs of schizophrenia, treatment, and management of schizophrenia patients; and 4 questions related to methods used to confirm diagnosis, referrals used, and medications prescribed to schizophrenia patients. All answers were marked as either correct (score=1) or incorrect (score=0). Demography was assessed with questions regarding gender; number of patients treated annually; patient consultation time; number of schizophrenia cases identified annually; and their continuing medical education (CME) experiences.
Knowledge was defined as the ability of the GP to correctly identify the symptoms of schizophrenia; its related treatments and to make appropriate referrals. Similarly, practice was defined as the ability of the GP to correctly indicate practice in diagnosing, treating and referring schizophrenia patients appropriately. The level of knowledge on schizophrenia diagnosis and treatment was assessed with two multi-item questions (K1: Which of the following do you think are the most frequent symptoms of schizophrenia? and K3: What is the ideal therapy for a first episode suspected case of schizophrenia?) and five other questions related to early warning signs of schizophrenia; antipsychotic medication use and its side effects; and estimation of the risk of relapse in untreated patients; (K2, K4-K7) with a maximum score of 19. A discriminating index was developed using the composite scores obtained by the practitioners\' responses to all (K1 through K7) Knowledge questions. Good Knowledge was defined as a composite knowledge response score of >12 (60% correct answers) and Poor Knowledge was defined with a composite knowledge score of <12 (below 60% correct answers).
In terms of practice, the experience of GPs with schizophrenia diagnosis, treatment and referrals was assessed with four multi-item questions (P1: How do you confirm schizophrenia diagnosis? P2: Do you treat schizophrenia patients at your clinic or in collaboration with other specialists in hospitals? P3: What medications do you prescribe for patients with first episode of schizophrenia? and P4: How do you describe the prognosis for a first episode schizophrenia patient who has received treatment?), with a maximum score of 22. A similar discriminating index using the composite scores obtained by the practitioners\' responses to all (P1 through P4) the Practice questions were developed. Adequate practice was defined as a composite practice response score of >13 (60% correct answers), and Inadequate practice was defined with a composite practice response score of <13 (below 60% correct answers).
The questionnaires were distributed to all GPs at their private clinics in Peshawar district. The completed questionnaires were collected by the investigator from the clinics at a later date.
The collected data was analyzed using Epi Info Statistical software. Demographic variables were analysed using frequencies and percentages. Proportions were calculated using the discriminating index of composite scores for Knowledge and Practice of the GPs. Student t test was used to compare the scores of GPs who treated and did not treat schizophrenia patients.
Results
There were 135 registered GPs invited to participate in this study, in that 114 (84.44%) consented to participate, while 21(15.56%) declined. The reasons given for non-participation were: "I have a busy schedule" 13(61.9%); "I don\'t see patients with schizophrenia" 6(28.6%); and "I don\'t want to fill the questionnaire" 2(9.5%).
Overall, 111(97.4%) GPs were males. A total of 46(40.4%) GPs reported never seeing any suspected cases of schizophrenia; 27(23.7%) suspected more than 5 cases of schizophrenia annually; 61(53.5%) never treated schizophrenia patients in their practice; 15(13.2%) treated more than 10 patients annually; and 7(6.1%) GPs indicated having received CME regarding schizophrenia.
The mean knowledge score was 8.48±3.27. The frequent symptoms of schizophrenia were identified correctly by 36 (31.5%) (a response score >5.4 which is >60% correct responses) GPs (Figure-1).
Besides, 71 (62%) GPs considered that the first episode of schizophrenia is preceded by early warning signs and estimated the relapse risk of untreated patients during the first year after a first schizophrenic episode to be more than 60 per cent. Only 15 (13.2%) considered giving antipsychotic medication for 12-24 months after a first schizophrenic episode and 14.0% considered giving it for 3-5 years for maintenance therapy in patients with multiple episodes of illness after the remission of an episode.
Only 6 (5.3%) GPs could name two side effects and 25 (21.9%) reported one side effect while 83 (72.8%) could not report any side effect of antipsychotic medication. Extra-pyramidal symptoms were the most relevant side effect reported by 27 (23.7%) GPs followed by weight gain reported by 4 (3.5%).
Good knowledge on schizophrenia diagnosis and treatment was found in 14 (12.3%) GPs with a composite score greater than or equal to 12 assessed on seven knowledge question (K1-K7) (Figure-2).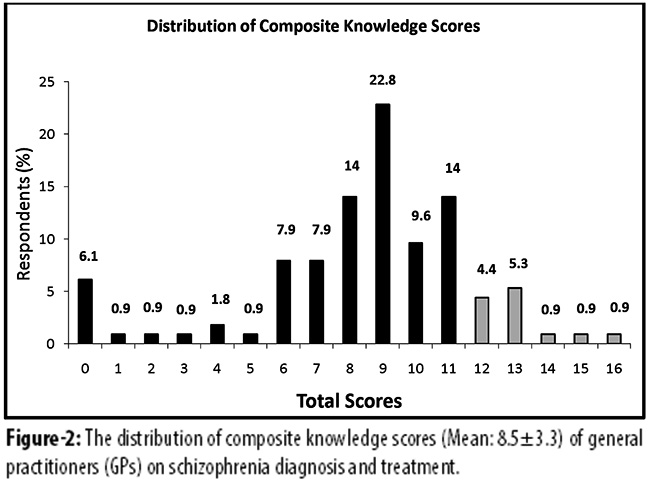
The annual experience of GPs with schizophrenia diagnosis, treatment and referrals was assessed with four multi-item questions (P1- P4). A mean composite score of responses to all four questions was 10.3±4.4. Adequate practice scores were found in 32 (28.1%) GPs (composite practice score of >13 which represents a >60% correct responses) (Figure-3).
A good proportion 87 (76.3%) of GPs relied on personal history and observation over several months for the confirmation of the diagnosis of schizophrenia. About 68 (59.6%) GPs preferred treating the patients exclusively in their clinic, while 45 (39.5%) considered referral to a specialist/psychiatric out-patient department (OPD) in a hospital with a complete handover of patient for treatment. Only 3 (2.6%) GPs could name four medications with their average doses, while 66 (57.9%) were not able to name any medication for the treatment of schizophrenia. The prognosis of a treated patient after a first episode of schizophrenia with a possibility of maintenance of performance level was correctly identified by 43 (37.7%) GPs.
In terms of association between Knowledge and Practice scores of those GPs who were treating schizophrenia patients versus those who were not showed significant difference (Table).
Discussion
International multicentre survey of GPs indicates that the mean numbers of patients with chronic schizophrenia seen by GPs are similar across many countries and healthcare systems.18 Most GPs are currently treating a small number of patients (on average about three patients) with schizophrenia which is similar to our finding where only 13.2% (n=15) treated more than 10 patients annually compared to 53.5% (n=61) GPs who didn\'t treat any diagnosed case of schizophrenia in a year, making almost two patients on average.19-21
The knowledge and skills of GPs about psychiatric disorders is generally poor and it is reported that 40-50% of GPs routinely screen patients for mental health issues, but depression is often not detected.22 It is perhaps not surprising that schizophrenia is often not diagnosed and we found that more than one-third of GPs didn\'t diagnose any new case in a year\'s time.
In our study, only 6.1% GPs received CME, an essential ingredient to maintain competence, regarding schizophrenia which, however, is slightly better than none reported in a study, but far less than the 30.8% reported in another study from Pakistan.21,23
Only 12.3% GPs in our sample had adequate knowledge about schizophrenia which visibly speaks about the current state of affairs regarding medical education in Pakistan and is in contrast with the findings of a French study where GPs had a fair theoretical knowledge of schizophrenia symptoms.24 However, the results related to knowledge are similar to another study conducted in a less developed semi-rural location which is contrary to what we expected considering the fact that our sample was from a provincial capital where abundant professional development opportunities and competition exist.
As compared to the figures reported by the Swiss and a local study (62% and 64% respectively),15,21 hallucinations and delusions were considered the most frequently experienced symptoms of schizophrenia by 81.6% GPs in our sample. However, bizarre behaviour which was considered by 56% in the Swiss study15 was considered by only 45.2% GPs in our sample.
GPs in our sample (62.3%) considering that the first episode of schizophrenia is preceded by early warning signs were much less than the Swiss study (90%) but comparable to another local study (69%).15,21 General practice is the first stop for any patient considering diagnosis and treatment for their health issues; our results show the unpreparedness of GPs who encounter patients of schizophrenia.
Pharmacotherapy, alone or in possible combination with other types of therapy, was considered ideal treatment by 88% GPs in the Swiss sample and 60% in another study.15,21 Our results were in between the two, where 70.2% GPs considered pharmacotherapy to be ideal.
Only 13.2% and 14% GPs of our sample were able to answer correctly the duration of antipsychotic medication to be maintained for more than 12 months after first schizophrenic episode, and for at least 3 years in patients with multiple episodes of illness after remission.25 Figures of 12.5% and 39% were reported for the same in a similar study.21 It is distressing to know as this suggest that even those patients who are diagnosed as cases of schizophrenia may receive incomplete treatment regime, leading to more chances of relapse.
Regarding their practices, the answers given to the questions in the questionnaire may not assess their actual practice, but should be considered more of a proxy measure.26 Only 20.2% (n=23) GPs had adequate practice in the management of schizophrenia. This percentage was much less than the percentage of any Practice question answered by GPs in a similar study conducted in Switzerland.15
In our sample, 76.3% GPs, each, relied on personal history and observation over several months for the confirmation of the diagnosis of schizophrenia, while GPs in the Swiss study showed more reliance on Information from others (65%) and family history (63%) respectively.15 The sample in another study relied more on personal history (87.5%) and family history (70%).21 All these serve as important diagnostic predictors of schizophrenia.27
Compared to 6.9% referrals to specialists, 39.5% GPs in our sample showed the same practice which though is much higher than that reported in the Swiss study,15 but is far less than the 60% reported in another study.21 However, 61.4% GPs were of the opinion of collaborating with the specialists which is comparable to 77.2% in the Swiss survey which is an encouraging finding.15
Antipsychotics (one or more) were mentioned as commonly used drugs for schizophrenia in their practice by 42.1% GPs which is far less than the figures reported in other studies (80% and 98.5%).15,21 A study from Pakistan reported that the problem in the rational use of psychotropic medication is due to the gaps in GPs\' knowledge about the management of mental disorders.23 This is an area of great concern as it poses serious questions not only on the practice but on the basic medical knowledge of these GPs.
The limitations of the current study should be kept in mind. The assessment of knowledge and practice was based on a cross-sectional view of the GPs\' responses to a questionnaire. The sample in this study may not be representative of all the GPs in Pakistan. The results of our study may not be generalisable to other settings as the training and role of GPs may vary in the international healthcare system.15 However, we had a good response rate and were able to contact most of the GPs working in Peshawar. Majority of respondents were male GPs. This perhaps reflects limited number of female doctors who limit themselves to providing obstetric services.
Although there are studies on evaluation of the training programmes for GPs7,28 but we believe this is the first study assessing the knowledge and practice of GPs about schizophrenia in a completely urban district of a developing country.
It can be argued that it will be insufficient to improve knowledge and practices of GPs only through educational programmes. In addition, synchronised provision of specialised services and assessment facilities for GPs may prove to be more important.15 From the GPs\' point of view, communication between the specialist and primary care services has been poor and problematic with unclear individual roles and responsibilities, while treating patients with schizophrenia and this may appear to be the biggest hindrance in service provision.14,19
Since it has already been established that rapid social integration can be achieved if the follow-up of patients with schizophrenia is arranged in general practice, the role of GP for dealing with somatic symptoms of the illness and renewing/changing their antipsychotic medication can\'t be emphasised more.29,30 This will definitely lead to a much needed collaborative care approach.29,31-33
The use of universal screening by all GPs is needed to improve detection rates of schizophrenia for which brief standardised screening questionnaires might be very useful, as suggested by GPs during the data collection meetings with them.14,22,34,35
Conclusion
Knowledge and practice of GPs related to schizophrenia diagnosis and treatment in Peshawar district, a major urban area, were poor. This may be one of the contributory factors for delayed diagnosis and perhaps inadequate treatment of schizophrenia patients. Education and training for GPs in the diagnosis and treatment of schizophrenia need to be improved significantly through outcome-based mental health education. Also, communication between mental health services provided by public health institutions and GPs needs particular improvement to improve access to mental health services for patients and to enable knowledge-sharing among GPs.
Acknowledgement
The study is based on a thesis/dissertation of the primary author, for MS (Mental Health Policy and Services), awarded by the Faculty of Medical Sciences, Department of Mental Health, NOVA University of Lisbon, Portugal, in 2013. It was done under the supervision of the second author.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington DC: American Psychiatry Association; 1994, pp 285.
2. World Health Organization: Schizophrenia. [Online] 2012 [Cited 2012 March 12]. Available from: URL: http://www.who.int/mental_health/ management/schizophrenia/en/.
3. Department of Community Health Sciences, Aga Khan University: Assessment of Health Status & Trends in Pakistan [Online] 2001 [Cited 2012 April 15]. Available from URL: http://www.aku.edu/SiteCollectionImages/AKU/zzchs/pdf/HealthSituationandTrend-Pakistan,2001.pdf.
4. Health care reform for Americans with severe mental illnesses: Report of the National Advisory Mental Health Council. Am J Psychiatry. 1993;150:1447-65.
5. Barbato A. World Health Organization: Schizophrenia and public health. [Online] 1998 [Cited 2012 January 15]. Available from: URL: http://www.who.int/mental_health/media/en/55.pdf
6. Murray CL, Lopez AD. The global burden of disease. Cambridge: Harvard University Press; 1996.
7. Oud MJ, Schuling J, Slooff CJ, Meyboom-de Jong B. How do General Practitioners experience providing care for their psychotic patients? BMC Fam Pract. 2007; 8: 37.
8. Parkes CM, Brown GW, Monck EM. The general practitioner and the schizophrenic patient. Br Med J. 1962 ;1:972-6.
9. King M, Nazareth I. Community care of patients with schizophrenia: the role of the primary health care team. Br J Gen Pract. 1996;46:231-7.
10. Taj R, Khan S. A study of reasons of non-compliance to psychiatric treatment. J Ayub Med Coll Abbottabad. 2005;17:26-8.
11. Copolov DL. Psychoses: a primary care perspective. Med J Aust. 1998;168:129-35.
12. Gadit AA. Psychiatry in Pakistan: 1947-2006: A new balance sheet. J Pak Med Assoc. 2007; 57:453-63.
13. Lang FH, Johnstone EC, Murray GD. Service provision for people with schizophrenia. II. Role of the general practitioner. Br J Psychiatry. 1997 ;171:165-8.
14. .Skeate A, Jackson C, Birchwood M, Jones C. Duration of untreated psychosis and pathways to care in first-episode psychosis: investigation of help-seeking behaviour in primary care. Br J Psychiatry Suppl. 2002; 43: s73-7.
15. Simon AE1, Lauber C, Ludewig K, Braun-Scharm H, Umbricht DS; Swiss Early Psychosis Project. General practitioners and schizophrenia: results from a Swiss survey. Br J Psychiatry. 2005; 187:274-81.
16. Farooq S. Never treated schizophrenia in developing countries. J Pak Psych Soc. 2008;5:53-4.
17. Heyrman J, Spreeuwenbergh C. Vocational training in general practice. Leuven: Katholieke Universiteit Leuven; 1987.
18. Simon A, Umbricht D, IGPS Group. Early psychosis in primary care: implications of the international GP study (IGPS) on service development. Schizophr Res 2004; 70:38-9.
19. Carr VJ, Lewin TJ, Barnard RE, Walton JM, Allen JL, Constable PM, et al. Attitudes and roles of general practitioners in the treatment of schizophrenia compared with community mental health staff and patients. Soc Psychiatry Psychiatr Epidemiol. 2004;39:78-84.
20. Lewin TJ, Carr VJ. Rates of treatment of schizophrenia by general practitioners. A pilot study. Med J Aust. 1998; 168:166-9.
21. Akhtar J, Haque M, Idress M, Awan NR, Irfan M. Knowledge and practice of general practitioners of Bannu about schizophrenia. J Postgrad Med Inst 2010;24:318-22.
22. Wang PS, Berglund P, Kessler RC. Recent care of common mental disorders in the United States: prevalence and conformance with evidenced-based recommendations. J Gen Intern Med. 2000; 15:284-92.
23. Naqvi HA, Sabzwari S, Hussain S, Islam M, Zaman M. General practitioners\' awareness and management of common psychiatric disorders: a community-based survey from Karachi, Pakistan. East Mediterr Health J. 2012; 18:446-53.
24. Verdoux H, Cougnard A, Grolleau S, Besson R, Delcroix F. A survey of general practitioners\' knowledge of symptoms and epidemiology of schizophrenia. Eur Psychiatry. 2006;21:238-44.
25. Practice guidelines for the treatment of patients with schizophrenia. American Psychiatric Association. Am J Psychiatry 1997;154:1-63.
26. Penn DL, Corrigan PW. The effects of stereotype suppression on psychiatric stigma. Schizophr Res 2002;55:269-76.
27. Mc Gorry PD, Mckenzie D, Jackson HJ. Can we improve the diagnostic efficiency, and predictive power of prodromal symptoms for schizophrenia? Eur Psychiatry. 2006; 21:238-44.
28. Oud MJT, Schuling J, Slooff CJ, Groenier KH, Dekker JH, de Jong BM. Care for patients with severe mental illness: the general practitioner\'s role perspective. BMC Fam Pract. 2009; 6:10:29.
29. Norton JL, Rivoiron-Besset E, David M, Jaussent I, Prudhomme C, Boulenger JP, et al. Role of the General Practitioner in the care of patients recently discharged from the hospital after a first psychotic episode: Influence of length of stay. Prim Care Companion CNS Disord. 2011;13. pii: PCC.11m01180.
30. Capdevielle D, Ritchie K. The long and the short of it: are shorter periods of hospitalisation beneficial? Br J Psychiatry. 2008; 192:164-5.
31. Dietrich AJ, Oxman TE, Williams JW Jr, Schulberg HC, Bruce ML, Lee PW, et al. Re-engineering systems for the treatment of depression in primary care: cluster randomised controlled trial. BMJ. 2004; 329:602.
32. Gilbody S, Whitty P, Grimshaw J, Thomas R. Educational and organizational interventions to improve the management of depression in primary care: a systematic review. JAMA. 2003; 289:3145-51.
33. Upshur C, Weinreb L. A survey of primary care provider attitudes and behaviors regarding treatment of adult depression: what changes after a collaborative care intervention? Prim Care Companion J Clin Psychiatry. 2008; 10:182-6.
34. Beck AT, Steer RA. Manual for the revised Beck Depression Inventory. San Antonio, Texas: Psychological Corporation; 1993.
35. Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967; 6:278-96.
Related Articles
Journal of the Pakistan Medical Association has agreed to receive and publish manuscripts in accordance with the principles of the following committees:




